
How Automation Makes Healthcare Payments More Human
With pre-authorization requirements on the rise, technology is delivering elevated and expedited experiences for patients and providers.
Most people who have visited a doctor’s office are familiar with “white-coat syndrome”—the phenomenon of blood pressure reading higher in a doctor’s presence than it does when a patient is at home.
But there’s no term to describe the anxiety that spikes when a patient’s care is thrown off course by a health insurance denial when seeking prior authorization—an all-too-common obstacle that requires approval from a health insurance plan before a patient receives care. Patients face a gut-wrenching decision: Will they appeal the decision and delay care, opt to pay out of pocket or back out of the procedure altogether?
The challenge is top of mind for Candice Hoshi, Vice President, Revenue Cycle for UCHealth, a Colorado-based nonprofit integrated health system with 12 hospitals and more than 150 UCHealth-owned and -affiliated clinics serving patients in Colorado, Wyoming and Nebraska.
Hoshi says that the challenges of the authorization process plague patients and providers alike, costing valuable time and money, and are invasive to every health system’s primary objective: to improve lives.
Insurance and billing should be unobtrusive elements of the patient experience, Hoshi says. But authorization requirements are only getting more extensive; in a recent Medical Group Management Association survey, 79% of medical practices reported that insurers’ prior authorization requirements had risen in the past year. The task of navigating the system is a herculean one, and health staff can’t—and in Hoshi’s view, shouldn’t—handle it alone.
Enter: smart automation.
The value of a human touch
Hoshi touts the value of freeing up healthcare workers to focus more on people-to-people interactions, rather than on the nitty-gritty of authorization processes that allow patients to receive care—and artificial intelligence and robotic process authorization (RPA) are making this prioritization possible.
“I want to be sensible about using our resources,” says Hoshi. “We have to make smarter decisions about when we use people—and I’d rather have people solving problems and interacting with patients if tech can replace other work.”
With the help of automation, hospitals and health systems are removing obstacles—like authorizations—to advance care and provide a better patient experience. Providers no longer need to manually look up authorization rules, fax approval request forms or physically follow up with phone calls or website checks.
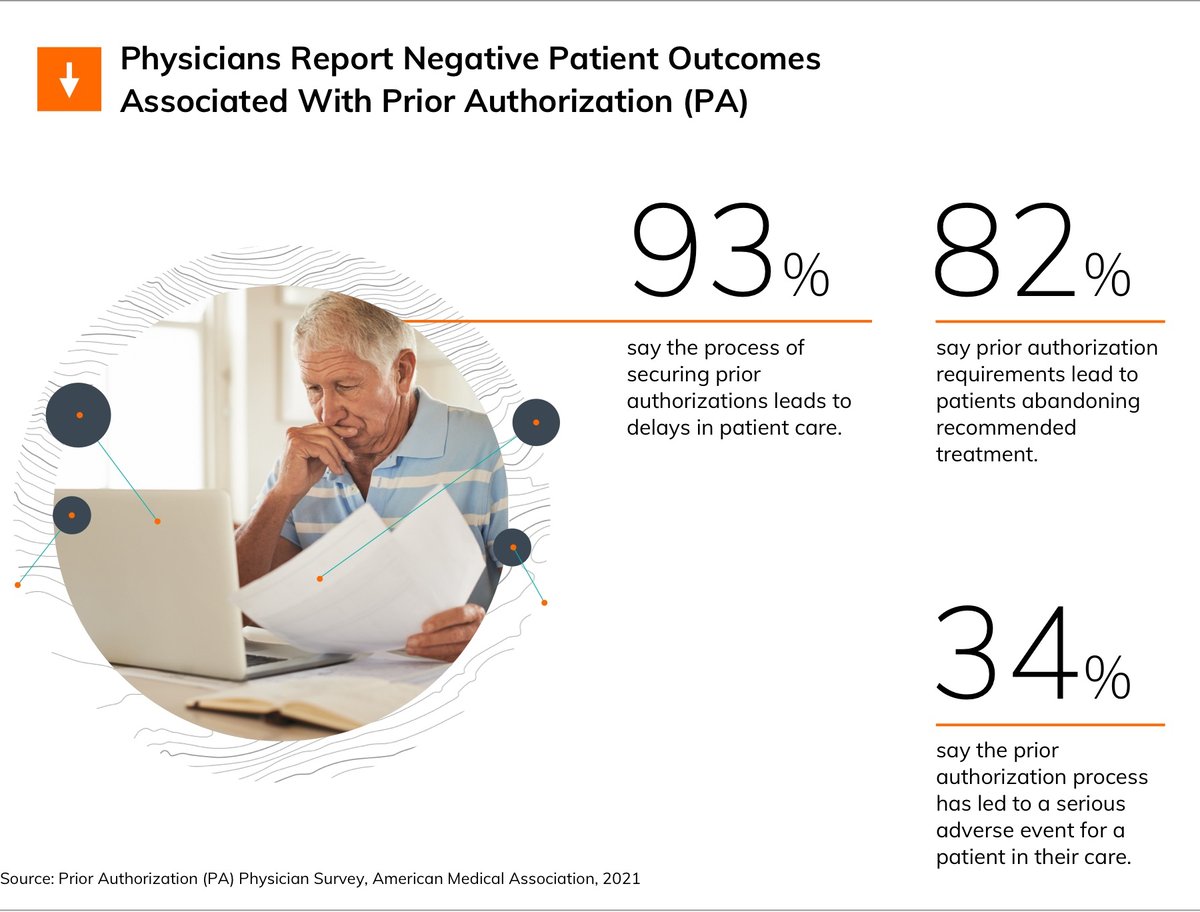
The change is a powerful one. According to the American Medical Association, physicians report that the challenges of prior authorization pose major impediments to patient care, and streamlining the process can help health systems better serve their communities.
After enhancing its revenue cycle management with AI from Waystar, UCHealth was able to speed up its authorization process, moving from handling authorizations just a few days before treatment to tackling them approximately two weeks in advance.
The shift has not only increased the health system’s capacity for processing authorizations, but has also led to a 46% reduction in denials. In cases where a denial is firm, healthcare workers have the time to connect with patients to ensure that their needs are met.
“We’ve optimized our workflow so that Waystar technology pulls the information from the physician order seamlessly to initiate an authorization on the payer website, statuses it and then pulls the information back into our electronic health record,” Hoshi explains. “It’s a really slick workflow. That means when an authorization cannot be secured, we have two weeks to have that conversation with the patient and can potentially redirect them to a different site of care, or they can choose to make an informed decision about paying out of pocket.”
Volume and complexity make smart automation mission-critical
High patient volume makes revenue cycle automation a transformative upgrade for a system like UCHealth, which treated a total of 2.7 million patients in 2022. Those 2.7 million patients can amount to an average of up to 7,400 insurance authorizations per day, and the complexity of different payer requirements and processes makes it all but impossible for staff to process these requests in a consistent and timely way.
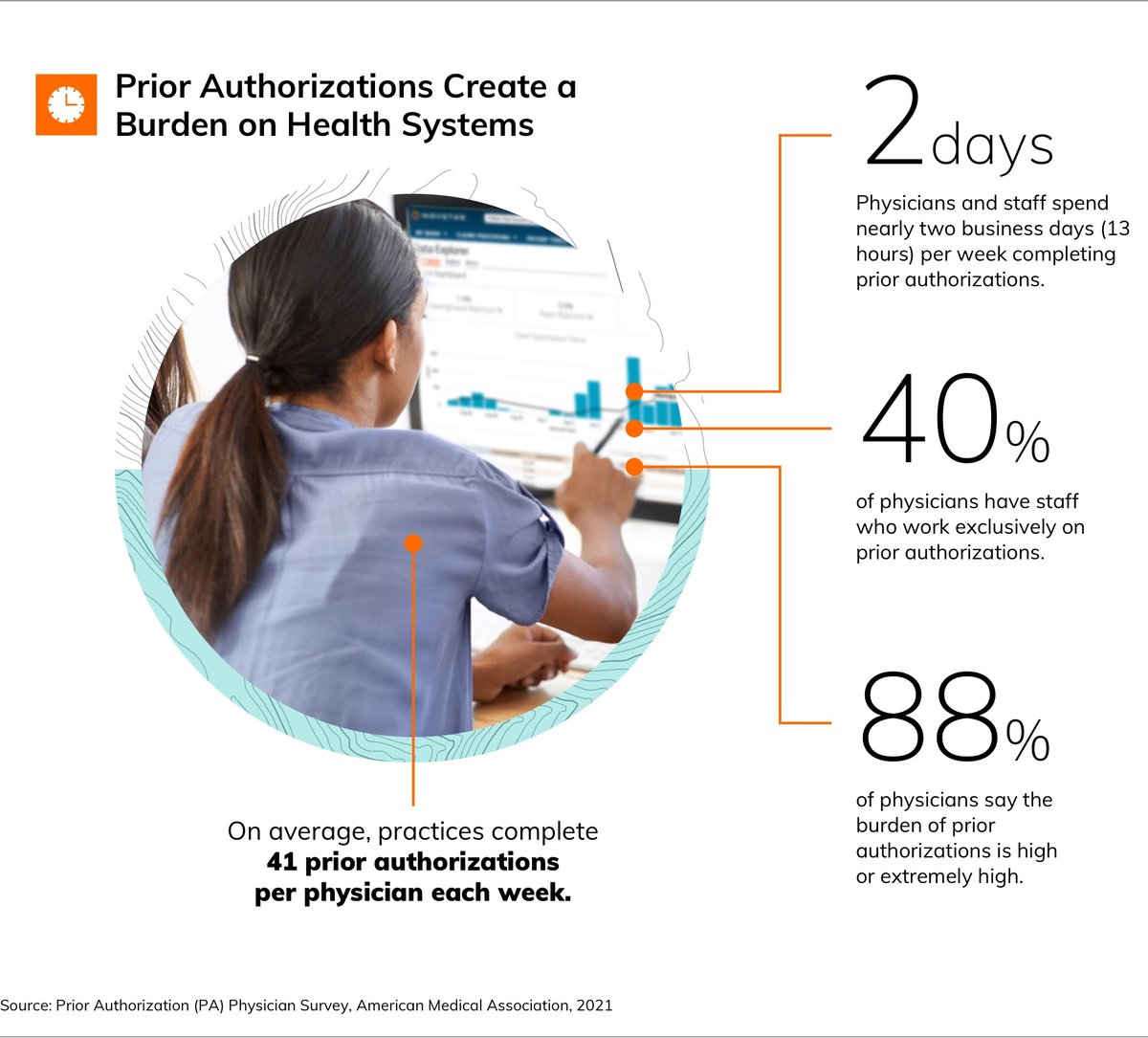
The intensifying burden of authorizations on healthcare workers has fueled growing adoption of machine learning and RPA in healthcare revenue administration. Today, half of US healthcare providers have invested in some form of RPA, according to an analysis by Gartner. The same report found that 20% of all patient interactions now involve some form of AI enablement.
UCHealth is one of many of the nation’s top health systems that have turned to Waystar’s AI tools to streamline and unify healthcare payments so that they can prioritize important people-to-people work for staff. The cloud-based Waystar platform integrates all major hospital information and practice management systems, processing more than $6 billion in patient payments annually and over 50% of claims for the US patient population with its technology.
Smart technology that works for healthcare administrative staff
At UCHealth, Hoshi and her team share Waystar CEO Matthew Hawkins’ patient-first mindset.
Hoshi is realistic about the workforce challenges facing the industry. With staff strapped by increased demands on health systems and a short supply of new recruits, she says that the pressure to leverage technology has never been higher—and all eyes are on automation-enabled solutions.
Since adopting the Waystar platform, 80% of prior authorizations now require no involvement from UCHealth staff, creating higher capacity for throughput, increasing time to solve complex cases and allowing increased focus on patient engagement.
“It’s very difficult to recruit skilled labor and to give them a sense of satisfaction, and now they aren’t burdened with having to keep up with the frenzied work they could never get ahead of,” says Hoshi.
In her view, the fruits of the AI-powered collaboration between UCHealth and Waystar can serve as a guidepost for the healthcare industry as it advocates for patients amid clinical and payment complexities that are unlikely to lessen anytime soon.
“We want the patient to remember the care that they got—not a billing issue or that their authorization created a barrier to getting what they need,” she says. “I challenge providers and payers alike to look at their own systems and address inefficiencies in service of allowing healthcare providers to provide the best care for their communities—and allowing them to get compensated for it.”
