How Artificial Intelligence Is Redefining the Patient Billing Experience
Smart payment platforms mean improved healthcare interactions
In today’s healthcare system, the billing office and the exam room often seem like they are in different zip codes. That’s because the disjointed healthcare payment process stands in stark contrast to the personal, caring nature of medicine. This clunky and confusing financial web involves providers, patients, employers and insurance companies, and often results in unexpected bills months after an appointment.
“The finance process often feels disconnected from the true patient healing process,” says Steve Burr, Senior Vice President, Revenue Cycle at Atrium Health, a nonprofit health system headquartered in Charlotte, N.C. that comprises 40 hospitals and more than 1,400 care locations in the Southeastern U.S.
To reconnect to that healing process, Atrium Health has invested in smart technology that’s changing how its finance team interacts with patients. Since doing so, Burr says his staff has seen a significant impact on their own work and on their interactions with patients. “We’re able to use technology behind the scenes to help eliminate paperwork so that patients can really focus on their treatments,” he says.
The push for greater price transparency
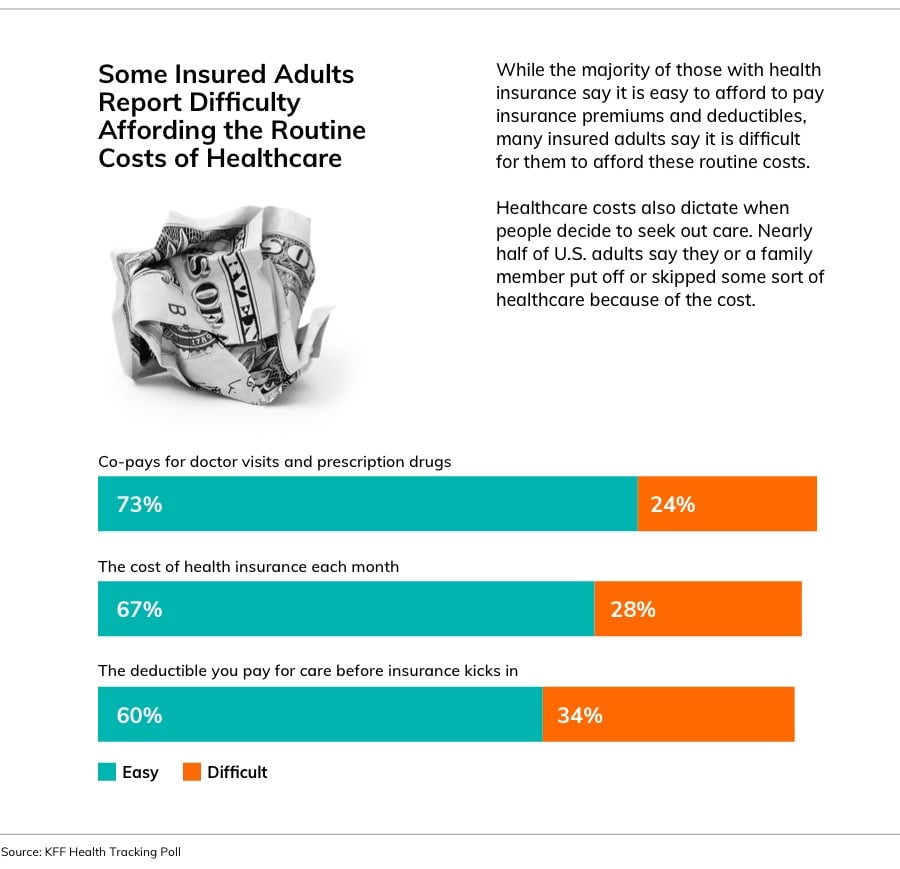
A recent survey by Kaiser Family Foundation found that two out of three U.S. adults worry that they won’t be able to afford a medical bill. It’s a fear embedded in the American psyche because the U.S. healthcare industry operates like no other, largely relying on manual processes to determine who owes what to whom, often well after the point of service. Typically, healthcare offices submit medical claims to insurers, await payment and then bill patients the amount remaining. Patients may receive confusing bills 60, 90 or even 120 days after an appointment, revealing costs they often didn’t anticipate.
While the industry is making strides to increase transparency (U.S. hospitals have been required to publish pricing information since the start of 2021) and cracking down on surprise billing (starting in 2022, the No Surprises Act will prohibit billing patients for unanticipated out-of-network charges), there’s still much room for improvement in healthcare billing.
Providers like Atrium Health use AI technology to simplify and unify healthcare payments, driving purpose-built automation across the revenue cycle. Atrium Health partners with Waystar to intelligently automate eligibility, authorizations, patient estimates, financial assistance and patient payments—helping to create a better financial experience for patients, while enabling providers to collect payments faster.
For patients, the result is knowing what they owe before receiving care. Say, for example, a man is concerned about his injured shoulder. His primary care doctor refers him to a community hospital run by Atrium Health for diagnostic services. The team at Atrium Health is enabled to quickly estimate the cost of treatment, including co-pays, co-insurance, insurance reimbursement rates and more. In advance of his appointment, they can tell him the price and offer to set up a payment plan.
“When a patient knows what to expect financially, it can improve the entire healthcare experience. Rather than worrying about unexpected bills showing up in their mailbox, they can turn all their attention to getting better,” says Matthew Hawkins, CEO of Waystar.
Intelligently automating administrative burdens
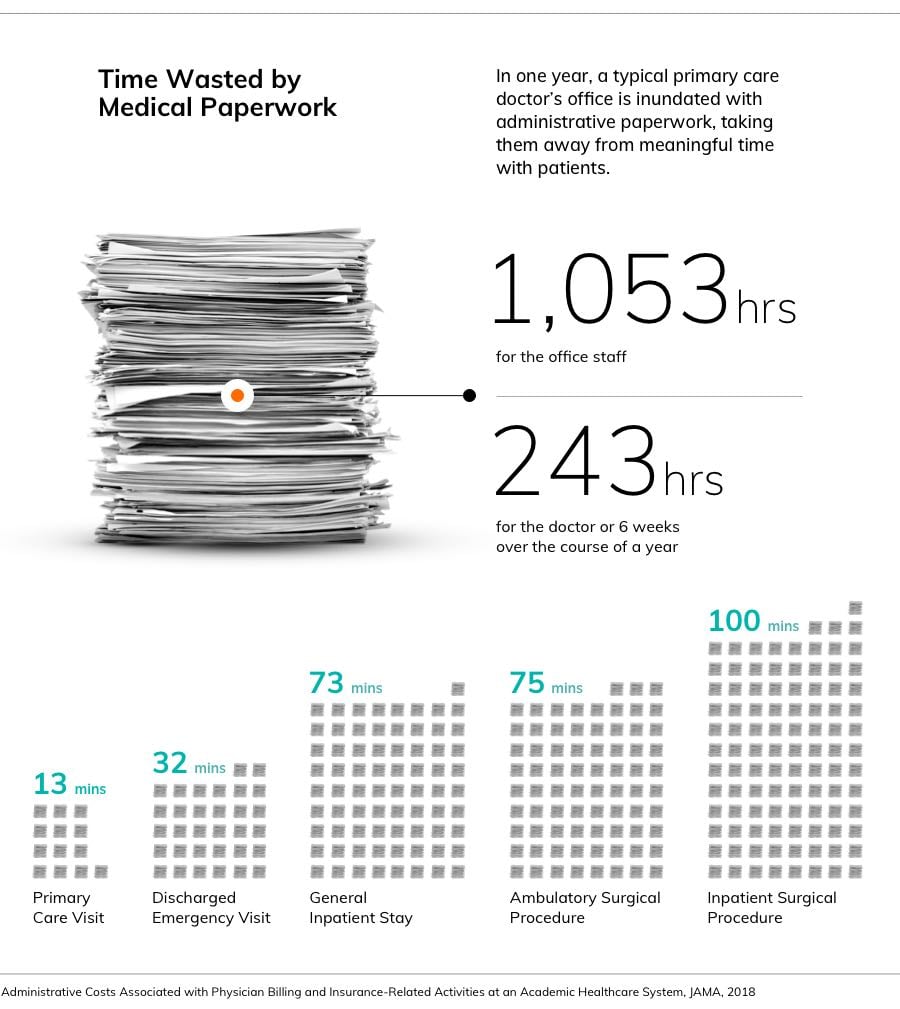
On average, physicians report that they spend more than 15 hours per week on paperwork and other administrative tasks, according to a 2021 Medscape report. Further, independent physicians say that reimbursement pressures are their biggest concern for staying in business.
In a busy hospital on any given day, an administrative team might need to verify the insurance policies of 1,000 patients and request insurance approval for hundreds of upcoming treatments and procedures. Any errors or failures to financially clear patients can have costly effects not only on the bottom line, but also on the patient experience. That’s why leading health systems like Atrium Health embrace Waystar’s AI and RPA (robotic process automation) capabilities to intelligently automate many cumbersome administrative tasks, so they can focus on what really matters most: their patients.
“We’ve been able to electronically complete a lot of [administrative] work, and do it on behalf of the patient. It is much easier for the patient to gain access to our system, as well as gain a better understanding of the financial policies we have in place,” says Burr.
Purpose-built automation is key to realizing immediate value for providers and patients. Many organizations still require patients to apply for financial aid and wait for staff to approve it. Atrium Health, on the other hand, uses Waystar’s AI technology to proactively identify patients eligible for financial assistance, freeing up staff to engage in compassionate, real conversations with patients about their treatments and their finances.
“It really helps our financial counseling team because they can process many more applications with the same number of staff, and, of course, it helps the patients because it’s a seamless process for the patient; it happens automatically. We get the Waystar score, which helps determine if the patient is eligible for financial aid, and the patient has to do nothing during that process,” says Chris Kiser, Vice President, Patient Financial Services–Patient Access at Atrium Health.
Burr says that Waystar’s technology has made a clear difference in how Atrium Health’s finance department works, and also in how the team sees its work.
At monthly meetings, team members dedicate the first few minutes to connect to their purpose by sharing success stories. Often, these come in the gracious words of patients who write thank-you letters to say they will never forget the help they received.“Please never underestimate how much mercy matters. You gave us a chance to continue to climb up instead of drowning in our circumstances,” one patient recently wrote.
It’s moments like those that remind Burr and his team why they chose to work in the healthcare industry.

“It’s about being there for people. By using technology to help with the paperwork, we can be fully present in those human moments that matter most.”
