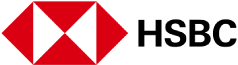
Turning Point: The Robotics Opportunity
What if we could use magnets to reach the deepest and most delicate parts of the human body, where no medical probe could go?
This was the challenge Pietro Valdastri found himself drawn to, first as a PhD student pursuing biomedical engineering in Pisa, and now as the founder of Science and Technologies of Robotics in Medicine (STORM) Lab in Leeds, a surgical robotics research lab dedicated to diagnosing and curing life-threatening diseases through minimally invasive solutions.
Take colon cancer: as the second deadliest form of cancer, the five-year survival rate plunges from around 95% if detected early to 11% in the later stages.
Colonoscopies are the gold standard for colon cancer detection, yet no major advancements beyond image quality have been made since the first fiberoptic endoscope was invented in 1957. Today, colonoscopies still involve inserting a stiff tube into the colon, are costly, and often painful enough to warrant full anesthesia.
Valdastri’s first foray into developing a minimally invasive colonoscopy solution dates back to his postdoctoral research in 2009, when working at the Institute of BioRobotics of Sant'Anna School of Advanced Studies on a European grant for the development of medical capsule robots. These are swallowed like a pill and enable imaging and intervention in the gastrointestinal tract.
Moving away from large, rigid robots and into the new territory of miniaturized, ingestible robots, Valdastri was part of a team that designed a capsule robot with 12 legs. This robot could “crawl” inside the intestine — inspired by the motion of insects.
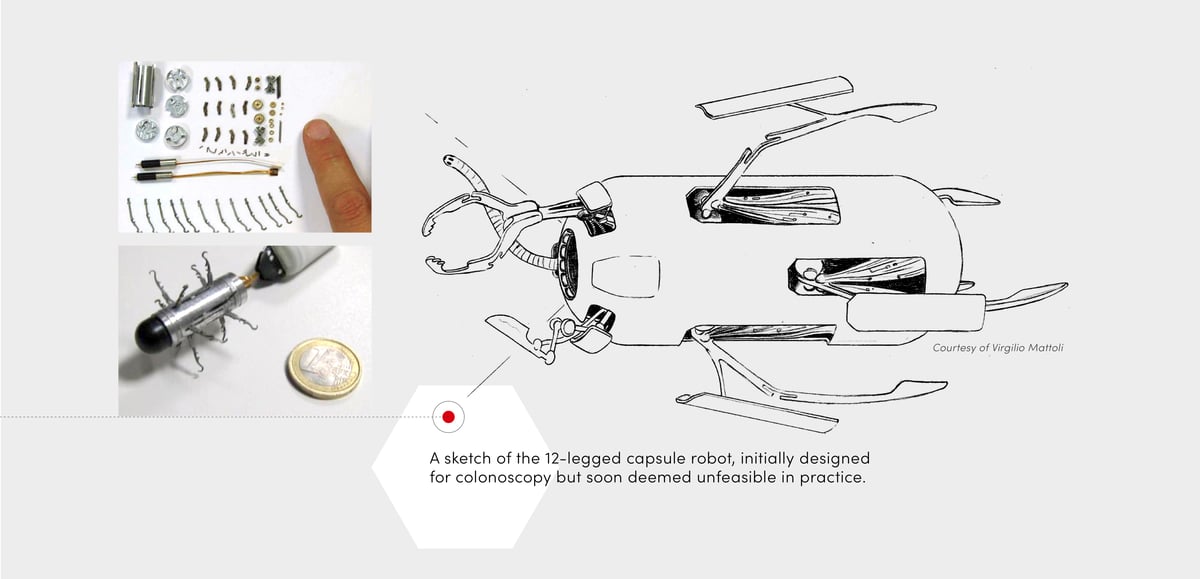
While this innovation received media attention and boosted Valdastri’s academic career, it proved “very ineffective in the clinical setting,” he reflects. Consisting of 72 micro-fabricated parts, the capsule robot was difficult to assemble and ran the risk of falling apart inside the body.
From that point, Valdastri decided to avoid blue sky ideas that could take decades to get from the lab to the patient. “I echo a colleague at ETH Zurich who’s only interested in developing ideas that can benefit patients during the course of his career. Having a clear picture of a clinical application is always our starting point now,” he says.

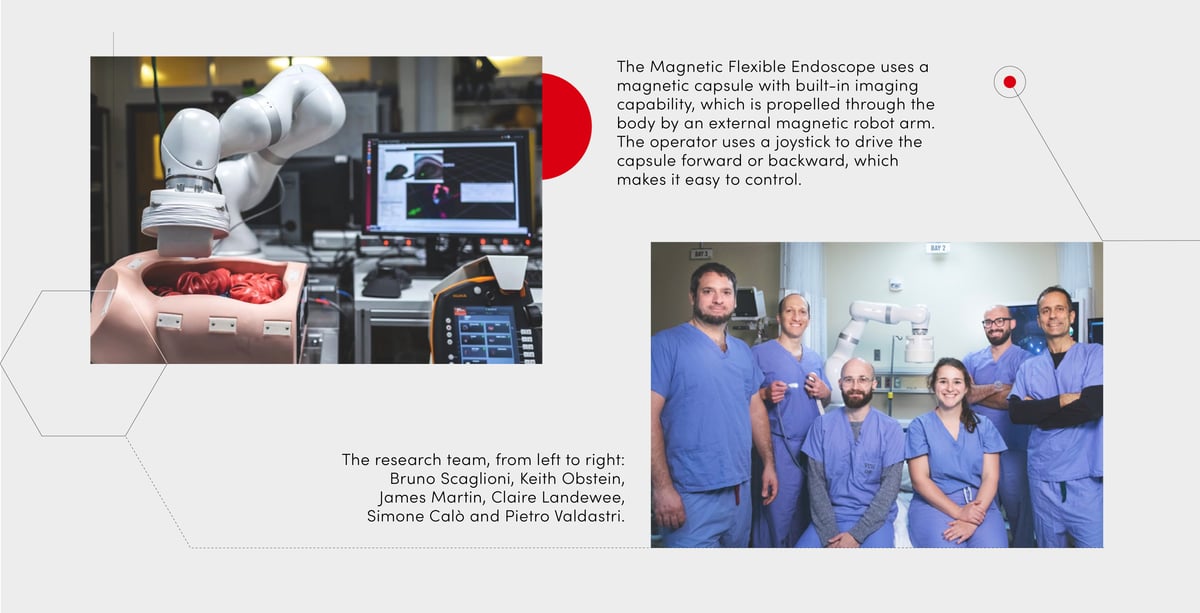
Casting aside that initial idea, Valdastri’s team began developing a more practical one: a robotic endoscope with a permanent magnet, controlled by an external arm. By using magnetic fields to intuitively guide the endoscope without stretching the patient’s tissue, more flexible, painless colonoscopy procedures were within reach.
“It costs about $15 to produce, so it’s disposable. The idea was to bring it to community centers, or places without extensive medical infrastructure, for colonoscopies to be performed there.”
But the team soon encountered a significant setback. While the magnetic endoscope could detect lesions, it was prone to losing magnetic coupling. “Without knowing where the tip of the magnetic endoscope was, the user had to go back to re-engage the magnet and try different directions,” explains Valdastri. “In the end, this was frustrating and three times slower than a conventional colonoscopy.”
The realization that any viable magnetic surgical technology relied on localizing the magnet in the human body in real time coincided with Valdastri’s move to Vanderbilt University in 2011.
When setting up STORM Lab — his first lab, Valdastri’s number one priority was selecting the right people. “A colleague told me: a PhD studentship lasts about four to eight years, which is similar to the length of some marriages. It’s important to select collaborators as you would select your partner for life,'” he says.
The enduring nature of STORM Lab’s partnerships is apparent in its ongoing work with its earliest collaborator: the gastroenterologist Keith Obstein, who also had a background in engineering. “He understood the technical challenges, while other clinicians sometimes didn’t get the engineering component. It's really important for engineers to speak as much as possible with doctors and vice versa, because we come from different end goals,” notes Valdastri.
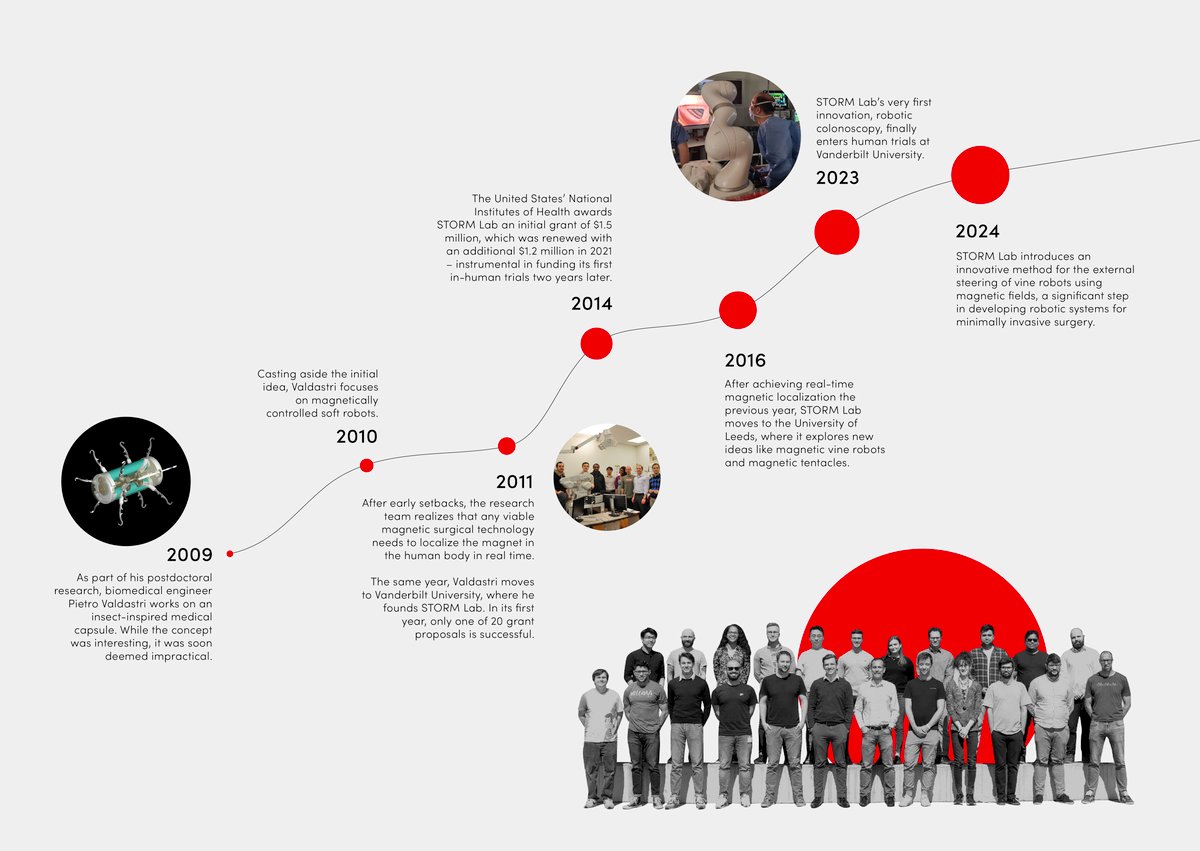
In STORM Lab’s first year, Valdastri learned resilience the hard way by writing around 20 grant proposals. Only one — fortuitously, the largest — was funded. “While you cannot take no as an answer, listening to feedback is just as important,” says Valdastri. “The good thing about the American system is that you get feedback, and then you can submit the proposal again. Every time you get feedback, you can improve.”
With that initial grant, STORM Lab was able to develop three iterations of its magnetic localization strategy, which is now the core technology underpinning its commercial spinoff, Atlas Endoscopy.

After 12 years in the making, and a move from Vanderbilt University to the University of Leeds along the way, STORM Lab’s very first innovation finally entered human trials in October 2023.
These milestone robotic colonoscopies, which Valdastri describes as his proudest moment, were led by Obstein, and made possible through industry partnerships. The loan of an ISO-certified robotic arm from German robotics manufacturer KUKA, for example, was crucial to STORM Lab's journey from bench trials to human trials.
After all patients reported no discomfort without sedation in phase 0 trials, Atlas Endoscopy is targeting FDA approval by 2026, and hopes to roll out its robotic endoscopes across the United States, China, Hong Kong and Europe.

Since settling at the University of Leeds, STORM Lab has focused on expanding beyond a single technology, and developing game-changing innovations like magnetic vine robots: a new class of robots with magnetic skin, which mimic the movement of creeping vines.
Developed in partnership with the University of California San Diego and the Korea Advanced Institute of Science & Technology, these robots have the potential to navigate S-bends and squeeze through the deepest parts of the lungs, beyond the reach of manual catheters.
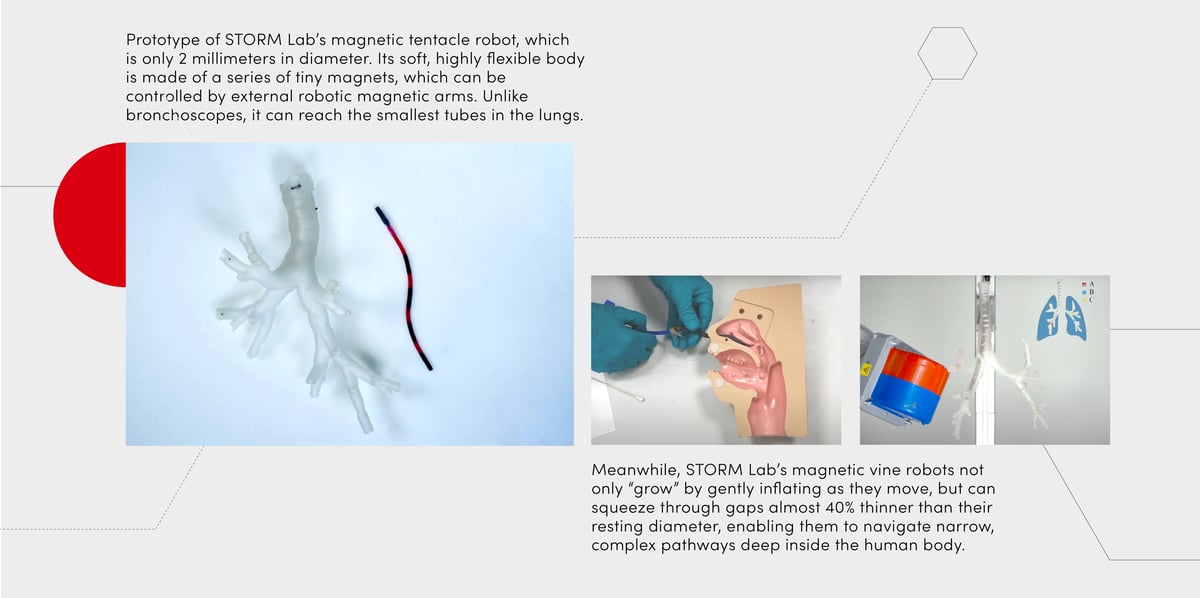
Beyond transforming patient outcomes for lung disease, STORM Lab’s vine robots could potentially diagnose and treat other life-threatening diseases, like brain tumors, without damaging the neurons in its path. “The dream would be to have a continuous pipeline of innovation that gets to patients,” says Valdastri.
“In 2007, I started a company that wirelessly monitors human health parameters like cardiac rate, ECG and blood pressure. We sold it to a larger company; it was big during Covid and is still in operation across Europe today. The highlight of my career is seeing my idea being used in hospitals. I’m really excited about the entrepreneurial cycle, and I want to do it again and again with the other technologies we have in the pipeline.”